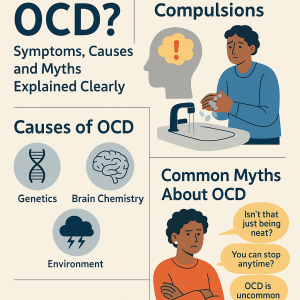
Types of OCD (Checking, Counting, Contamination, etc.): A Complete Guide
Types of OCD: Obsessive-Compulsive Disorder (OCD) is often misunderstood as simply being “too clean” or “a perfectionist.” In reality, OCD is a chronic mental health condition that manifests in diverse ways, affecting millions of people worldwide. From checking and counting compulsions to contamination fears and intrusive thoughts, OCD takes many forms—each with its own challenges.
In this article, we’ll explore the different types of OCD, how they impact daily life, and the treatment options available to help manage symptoms effectively.
Understanding Obsessive-Compulsive Disorder (OCD)
What is OCD?
OCD is a mental health disorder characterized by obsessions (intrusive, unwanted thoughts, images, or urges) and compulsions (repetitive behaviors or mental rituals performed to relieve anxiety). These patterns can consume significant amounts of time, disrupt daily functioning, and cause severe emotional distress.
Causes and Risk Factors of OCD
The exact cause of OCD remains unclear, but research suggests a mix of:
-
Genetics: Family history may increase risk.
-
Brain chemistry: Imbalances in serotonin and hyperactive brain circuits.
-
Environmental factors: Trauma, stress, or infections may trigger onset.
Symptoms of OCD Across Different Types
-
Repetitive checking (doors, stoves, locks)
-
Excessive handwashing or cleaning
-
Need for order, symmetry, or exactness
-
Intrusive thoughts of harm or taboo ideas
-
Mental rituals like silent counting or repeating phrases
The Main Types of OCD

Checking OCD
One of the most common subtypes, checking OCD is driven by doubts and fears of harm.
Common Checking Behaviors
-
Repeatedly ensuring doors are locked
-
Checking appliances to avoid fire hazards
-
Re-reading or re-writing to prevent mistakes
Triggers and Anxiety Patterns
People with checking OCD often feel intense responsibility for preventing harm, even when the risk is unrealistic.
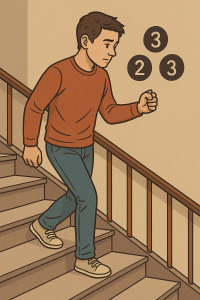
Counting OCD
This subtype involves compulsive counting rituals to neutralize anxiety.
Rituals and Mental Compulsions
-
Counting tiles, steps, or objects
-
Repeating tasks a specific number of times
-
Believing “bad things” will happen if a ritual isn’t completed
Everyday Life Impact
Counting OCD can make simple activities—like walking to work—exhausting and time-consuming.
Contamination OCD
This is perhaps the most stereotyped subtype, but it goes beyond fear of germs.
Fear of Germs and Cleanliness Rituals
-
Excessive handwashing or showering
-
Avoiding public spaces or touching shared objects
-
Fear of illness or spreading contamination
Emotional and Social Consequences
Contamination OCD often leads to isolation, strained relationships, and missed opportunities due to avoidance behaviors.
Symmetry and Ordering OCD
This subtype focuses on the need for exactness and balance.
Obsession with Perfection
-
Arranging items symmetrically
-
Fixating on even numbers or patterns
-
Repeating actions until they “feel right”
Organizing Rituals and Repetition
Such compulsions can dominate daily routines, making productivity nearly impossible.
Intrusive Thoughts OCD
This form is often invisible to others, as it centers on mental obsessions.
Harm-Related Intrusive Thoughts
-
Fear of accidentally hurting someone
-
Worrying about violent or sexual impulses
Religious (Scrupulosity) OCD
-
Excessive praying or confessing
-
Less Common Subtypes of OCD
While checking, counting, and contamination are among the most recognized forms, OCD can also manifest in less common but equally distressing ways.
Hoarding OCD
Unlike standard hoarding disorder, hoarding within OCD is usually tied to fearful obsessions.
-
Example: Keeping newspapers to avoid “losing important information.”
-
Impact: Living spaces can become unsafe and overwhelming.
Relationship OCD (ROCD)
This type focuses on doubts about relationships.
-
Constantly questioning if they love their partner enough.
-
Replaying conversations to check for reassurance.
-
Seeking validation about loyalty or compatibility.
Existential OCD
Here, obsessions revolve around deep philosophical questions:
-
“What if none of this is real?”
-
“What if I never find life’s purpose?”
These questions loop endlessly, creating anxiety and detachment from reality.
How OCD Differs from Normal Habits
OCD vs. Perfectionism
-
Perfectionism: Wanting to do things well for personal satisfaction.
-
OCD: Feeling compelled to repeat tasks out of fear something terrible will happen.
OCD vs. General Anxiety
-
General Anxiety Disorder (GAD) involves constant worry across situations.
-
OCD narrows into specific intrusive thoughts with compulsions to neutralize them.
Impact of OCD on Daily Life
Emotional and Mental Health Struggles
-
Constant feelings of fear, guilt, or shame.
-
Exhaustion from endless rituals.
-
Increased risk of depression or substance misuse.
Social, Work, and Family Life Effects
-
Missing school or work due to rituals.
-
Strained relationships when loved ones can’t understand behaviors.
-
Avoidance of social gatherings due to contamination fears or intrusive thoughts.
Diagnosis and Professional Help
How OCD is Diagnosed
-
Clinical interviews and history-taking.
-
DSM-5 criteria: Presence of obsessions, compulsions, or both, lasting at least an hour a day and impairing life.
Common Misdiagnoses
-
ADHD (due to restlessness).
-
Depression (due to low mood).
-
Autism spectrum disorders (due to repetitive behaviors).
A professional assessment is essential to receive the right treatment.
Evidence-Based Treatments for OCD
Cognitive Behavioral Therapy (CBT)
CBT helps patients challenge irrational beliefs and develop healthier coping strategies.
Exposure and Response Prevention (ERP)
The gold standard treatment for OCD, ERP gradually exposes individuals to triggers while preventing compulsions. Example: touching a doorknob without washing hands afterward.
Medication Options
-
SSRIs (Selective Serotonin Reuptake Inhibitors) like fluoxetine or sertraline.
-
Antipsychotics in severe or treatment-resistant cases.
Lifestyle Adjustments and Self-Help Strategies
-
Regular exercise to reduce anxiety.
-
Mindfulness and meditation to break obsessive loops.
-
Limiting caffeine and alcohol.
Living with OCD: Coping and Support
Daily Coping Mechanisms
-
Journaling obsessive triggers.
-
Setting small goals to gradually reduce rituals.
-
Practicing grounding techniques during intrusive thoughts.
Support Groups and Therapy Communities
-
Online forums and local support groups help reduce isolation.
-
Family therapy educates loved ones on how to respond without enabling compulsions.
(For more resources, visit International OCD Foundation)
FAQs on Types of OCD
Q1: Can a person have more than one type of OCD?
Yes, many individuals experience overlapping subtypes, such as checking and contamination OCD simultaneously.Q2: Is OCD caused by stress?
Stress doesn’t directly cause OCD but can trigger or worsen symptoms in people already predisposed.Q3: Can OCD go away on its own?
OCD rarely disappears without intervention. Treatment like ERP and medication is often necessary for long-term relief.Q4: Are intrusive thoughts normal?
Yes, most people have occasional intrusive thoughts. However, in OCD, these thoughts become persistent, distressing, and lead to compulsive rituals.Q5: What is the most severe form of OCD?
There isn’t a single “most severe” type. Severity depends on how much symptoms interfere with daily functioning. For some, contamination OCD is disabling; for others, intrusive thoughts can be more crippling.Q6: Is OCD the same as being neat or organized?
No. OCD is not about personal preference—it’s about overwhelming anxiety and uncontrollable compulsions.
Conclusion: Hope and Healing with OCD
OCD is a complex and often misunderstood disorder that extends far beyond stereotypes of cleanliness or perfection. From checking and counting to contamination fears and intrusive thoughts, each type presents unique challenges.
The good news? Effective treatments exist. With therapies like CBT and ERP, combined with medication and strong support systems, people with OCD can regain control of their lives.
If you or someone you know struggles with OCD, remember—you are not alone. Help is available, and with the right care, healing is possible.
Fear of blasphemy or moral wrongdoing
-