What is OCD? Symptoms, Causes and Myths Explained Clearly
Introduction to Obsessive-Compulsive Disorder (OCD)
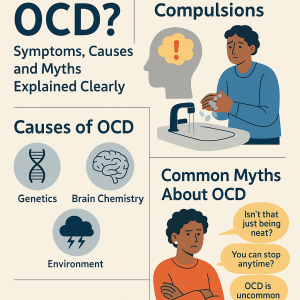
What is OCD. Obsessive-Compulsive Disorder, commonly known as OCD, is a mental health condition that affects millions of people worldwide. It is often misunderstood and surrounded by myths, which can prevent individuals from seeking proper help. In simple terms, OCD involves persistent, unwanted thoughts (obsessions) and repetitive behaviors (compulsions) that a person feels driven to perform.
Understanding what is OCD is essential because it goes beyond stereotypes of being “too neat” or “overly organized.” It can significantly disrupt daily life, relationships, and overall well-being if left untreated.
Obsessive-Compulsive Disorder A Clear Definition
OCD is classified as an anxiety disorder characterized by a cycle of obsessions and compulsions. These are not just habits like double-checking if the door is locked. Instead, they are intense, distressing, and time-consuming patterns that interfere with normal functioning.
The Difference Between Normal Habits and OCD
-
Normal Habit: Washing hands before eating.
-
OCD Compulsion: Washing hands repeatedly for hours, even when clean, due to fear of contamination.
The difference lies in intensity, frequency, and distress caused by the behavior.
How Obsessive-Compulsive Disorder Affects Daily Life
OCD can consume hours of a person’s day. For example, someone may avoid social activities because they’re stuck in cycles of checking, cleaning, or seeking reassurance. This can lead to isolation, stress, and lower quality of life.
Key Symptoms of Obsessive-Compulsive Disorder
Obsessions: Unwanted Thoughts and Urges
Obsessions are intrusive thoughts that cause anxiety. Examples include:
-
Fear of germs or contamination.
-
Doubts about safety (like leaving the stove on).
-
Intrusive, disturbing thoughts that go against one’s values.
Compulsions: Repetitive Actions and Behaviors
Compulsions are actions performed to relieve anxiety caused by obsessions. Common examples include:
-
Excessive handwashing or cleaning.
-
Counting, arranging, or repeating words.
-
Constantly checking doors, appliances, or locks.
Emotional and Physical Effects of This Disorder
-
High stress and fatigue.
-
Difficulty concentrating.
-
Sleep disturbances.
-
Feelings of guilt, shame, or frustration.
Causes of Obsessive-Compulsive Disorder: Why Does It Happen?
Genetic Factors and Family History
Research suggests that Obsessive-Compulsive Disorder can run in families, indicating a genetic link.
Brain Chemistry and Neurotransmitters
An imbalance in serotonin, a neurotransmitter that regulates mood, is thought to play a role in OCD.
Environmental Triggers and Stress
Traumatic events, chronic stress, or infections may trigger OCD symptoms in people who are already vulnerable.
Common Myths About Obsessive-Compulsive Disorder
Myth 1: Obsessive-Compulsive Disorder is Just Being Neat and Organized
Reality: OCD is not about simple preferences for cleanliness. Many people with OCD struggle with disturbing thoughts unrelated to cleaning.
Myth 2: People Can Simply “Snap Out” of Obsessive-Compulsive Disorder
Reality: OCD is a serious mental health disorder, not a bad habit. Treatment is often necessary.
Myth 3: OCD is Rare and Uncommon
Reality: OCD affects about 2–3% of the global population, making it far from rare.
Myth 4: Obsessive-Compulsive Disorder Only Affects Adults
Reality: OCD can begin in childhood and adolescence, making early detection vital.
Diagnosing Obsessive-Compulsive Disorder: What Doctors Look For
Clinical Evaluation and Tests
There’s no single test for OCD. Instead, doctors use interviews, questionnaires, and psychological assessments to evaluate symptoms. They focus on how much time obsessions and compulsions take up and how they impact daily life.
DSM-5 Criteria for OCD
According to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), OCD is diagnosed when:
-
A person experiences obsessions, compulsions, or both.
-
These behaviors are time-consuming (more than an hour per day).
-
Symptoms cause significant distress or interfere with work, school, or relationships.
Treatment Options for OCD
Cognitive Behavioral Therapy (CBT) and ERP
The most effective form of therapy for OCD is Cognitive Behavioral Therapy (CBT), particularly a technique called Exposure and Response Prevention (ERP). ERP helps people face their fears while resisting compulsive behaviors, breaking the cycle of OCD.
Medications for Obsessive-Compulsive Disorder
Doctors may prescribe medications like Selective Serotonin Reuptake Inhibitors (SSRIs) to help balance brain chemistry. These medications often reduce symptoms and make therapy more effective.
Lifestyle Changes and Support Systems
-
Practicing relaxation techniques (yoga, meditation, deep breathing).
-
Keeping a structured daily routine.
-
Seeking emotional support from friends, family, or support groups.
Living with OCD: Coping Strategies
Self-Care Practices for OCD
-
Journaling to track triggers.
-
Limiting caffeine and alcohol, which can worsen anxiety.
-
Prioritizing good sleep habits.
Support from Family and Friends
Loved ones can help by being patient, avoiding judgment, and learning about OCD to understand the struggles better.
Joining OCD Support Groups
Online and in-person support groups provide a safe space to share experiences and coping strategies. Organizations like the International OCD Foundation offer resources and community support.
Obsessive-Compulsive Disorder in Children and Teenagers
How Obsessive-Compulsive Disorder Shows Up in Kids
In children,Obsessive-Compulsive Disorder often presents as:
-
Repetitive rituals (like touching objects in a certain way).
-
Constant reassurance-seeking.
-
Extreme distress over “bad thoughts.”
Early Intervention Benefits
Getting help early can prevent Obsessive-Compulsive Disorder from worsening and improve long-term outcomes. Therapy adapted for children, combined with family support, often works best.
OCD vs Anxiety Disorders: Key Differences
While OCD is classified as an anxiety disorder, it has unique traits:
-
OCD: Focused on obsessions and compulsions.
-
General Anxiety Disorder (GAD): More about constant worry without compulsive behaviors.
-
Phobias: Triggered by specific fears rather than intrusive thoughts.
Understanding these differences ensures proper treatment and prevents misdiagnosis.
When to Seek Professional Help
Seek professional help if:
-
Obsessions or compulsions take more than an hour a day.
-
Daily life, work, or school is disrupted.
-
Stress, anxiety, or depression becomes overwhelming.
Early treatment leads to better management and long-term relief.
Frequently Asked Questions (FAQs)
1. Is OCD curable?
OCD is not “curable,” but it is highly treatable with therapy, medication, and coping strategies. Many people live full, productive lives with proper treatment.
2. Can stress make OCD worse?
Yes. Stress often intensifies OCD symptoms, making obsessions and compulsions harder to control.
3. Does OCD only affect adults?
No. OCD can begin in childhood, and early treatment is often key to reducing severity.
4. Are OCD medications addictive?
No. The most common medications, like SSRIs, are not addictive, though they may cause side effects.
5. Can someone have OCD and another mental health disorder at the same time?
Yes. OCD often coexists with depression, anxiety, or even ADHD. This is called comorbidity.
6. Is OCD the same as being a perfectionist?
Not at all. Perfectionism is a personality trait, while OCD is a medical disorder involving intrusive thoughts and compulsive behaviors.
Conclusion: Understanding Obsessive-Compulsive Disorder with Clarity
Obsessive-Compulsive Disorder is more than just a habit or personality quirk. It’s a serious mental health condition that can greatly impact daily life if left untreated. By debunking myths, understanding the symptoms, and exploring treatment options, we can foster awareness and empathy for those affected.
With therapy, medication, and strong support systems, people with Obsessive-Compulsive Disorder can manage symptoms and lead fulfilling lives. The key is early intervention, education, and compassion.